Basics of Medical Billing & Coding Online Course
Welcome to Free Medical Billing Training. Free practical lessons on the concepts and fundamentals of medical billing and coding. Just click on the topics below to start.
This is an abbreviated version of the Fundamentals of Medical Billing Course we developed to train new employees and contractors for our billing service.
This online course includes over 50 video lessons, 45 essential medical office forms, and downloadable copies of approximately 200 pages of presentation material.

Topic Covered in More Detail in our Online Fundamentals of Medical Billing Course

Welcome to the Basics of Medical Billing & Coding
Basics of Medical Billing & Coding Lessons
Lesson 1: What Is Medical Billing?
Lesson 2: Billing & Coding Terminology
Lesson 3: Health Insurance Plans
Lesson 4: Provider And Patient Setup
Lesson 5: Introduction To Medical Coding
Lesson 6: Creating And Submitting Claims
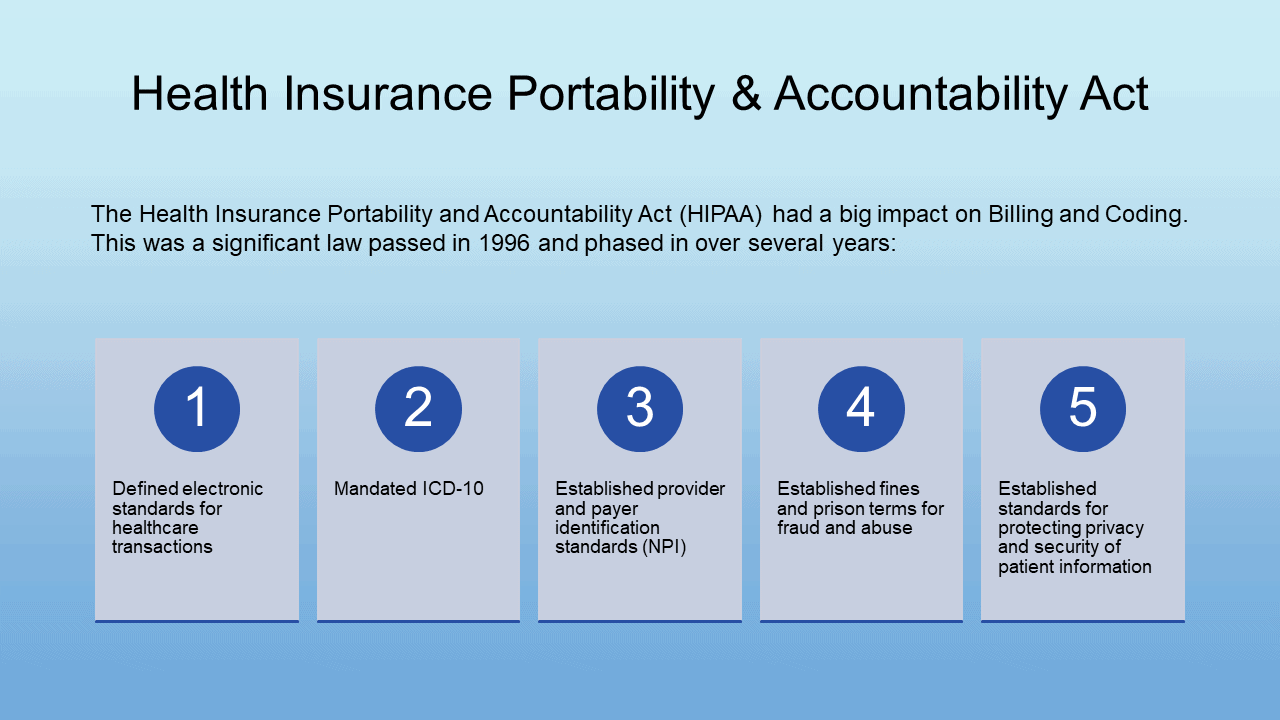
Lesson 7: Fraud Abuse And Privacy
Lesson 8: When Claims Don’t Get Paid
Lesson 9: Applying Payments
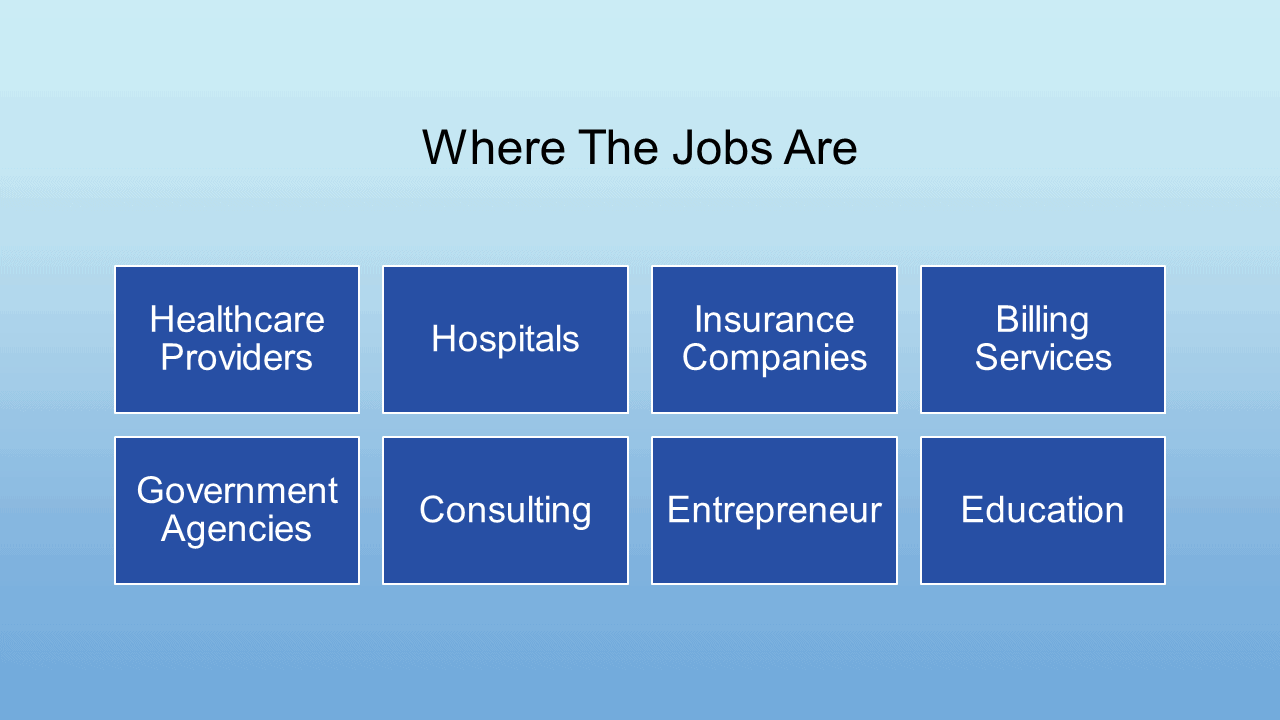
Lesson 10: Billing And Coding Career Options
Medical billing and coding is a process that involves the conversion of healthcare procedures and services into universal medical codes that can be used for billing and reimbursement purposes. Medical billing and coding professionals are responsible for accurately assigning these codes to healthcare services and procedures, ensuring that healthcare providers are reimbursed correctly and in a timely manner.
Medical coding involves the use of standardized codes to accurately represent medical diagnoses and procedures. There are several coding systems, including ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) for diagnosis codes, and CPT (Current Procedural Terminology) and HCPCS (Healthcare Common Procedure Coding System) for procedure codes. These codes are used to communicate important information about the patient’s medical condition and the services rendered to insurance companies, government agencies, and other payers.
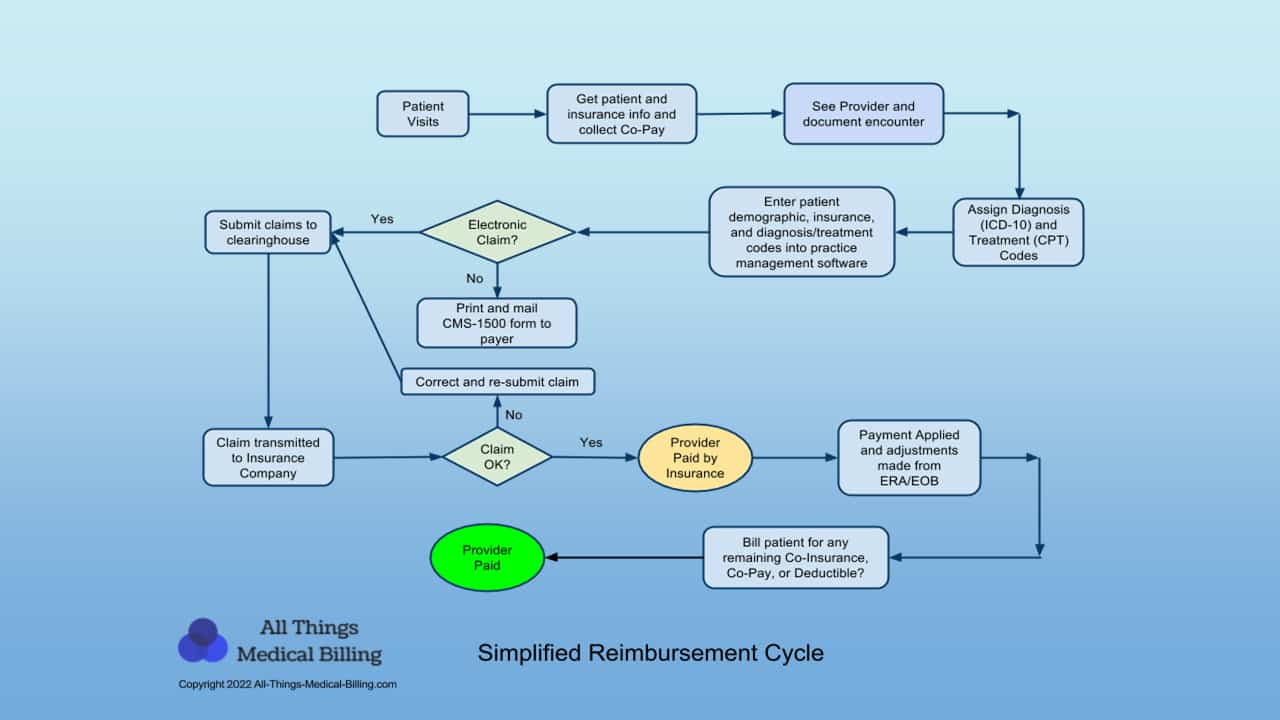
Medical billing involves the process of submitting claims to insurance companies or other payers to request reimbursement for healthcare services provided to patients. Medical billing professionals are responsible for verifying insurance coverage, ensuring that the correct codes are used for billing, submitting claims, and following up with payers to resolve any issues or disputes that arise.
Medical billing and coding professionals work in a variety of healthcare settings, including hospitals, clinics, physician offices, and insurance companies. They play a critical role in ensuring that healthcare providers receive proper reimbursement for their services, and that patients are not responsible for paying more than they should for their medical care.